The 7 Patterns Every Clinic Should Monitor Monthly
- Cale Queen
- Dec 8, 2025
- 4 min read
Metrics measure the past. Strategic signals reveal the future.
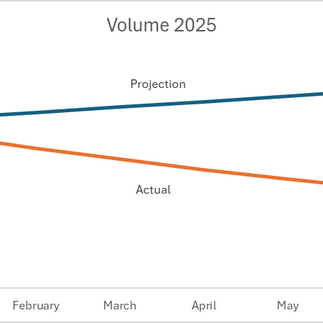
In Week 1, we saw how fast 2025 shifted beneath clinic owners.
In Week 2, we introduced the Assumption Gap — the space between what we thought the year would look like and what we actually lived through.
In Week 3, we built daily clarity with the By-Exception Briefing.
This week, we move to the monthly level.
Daily clarity keeps operations aligned. Monthly pattern recognition keeps your strategy aligned. Most dashboards show you what happened. Patterns show you what’s starting to change.
These seven patterns matter because they warn you when the world is drifting away from the assumptions that hold your plan together.
They show drift before it becomes damage.
Why Patterns Matter
Clinic plans rarely fail suddenly. They fail gradually — because early signals didn’t look urgent. Patterns reveal:
changes in access
shifts in payer behavior
rising patient complexity
signs of demand instability
early workflow strain
capacity stress
subtle signs of patient leakage
Seeing these early turns small adjustments into big advantages. Missing them forces you to react instead of lead.

The 7 Patterns Every Clinic Should Watch Monthly
Each pattern follows a simple structure: What it is → What to watch → Why it matters. This keeps the process disciplined and fast.
1. Access Delay (Third Next Available Appointment)
What it is: The MGMA/IHI standard for access. TNAA shows how long a patient actually waits to be seen.
What to watch:
TNAA creeping up for new or established patients widening gap between new vs. established patients
TNAA increased dependence on work-in slots
Why it matters: Rising TNAA weakens assumptions about demand, revenue, and retention. It signals misalignment between how patients seek care and how your schedule delivers it.
2. Payer Behavior Drift
What it is: Quiet changes in how payers edit, deny, or downcode claims.
What to watch:
more downcoding (especially Medicare Advantage)
new documentation phrasing requirements
repeated “insufficient documentation” denials
clean visits suddenly returning
Why it matters: When payer rules shift mid-year, your revenue model — and your plan — lose accuracy.
3. Case-Mix Complexity Shift
What it is: Changes in the complexity of the patients you’re seeing.
What to watch:
more multimorbidity
chronic care becoming dominant
longer visits/ routing visits over running scheduled time
rising behavioral/metabolic overlays
Why it matters: Complexity drives capacity, timing, staffing, reimbursements, and cycle time. If complexity shifts, everything else shifts with it.
4. Utilization Instability
What it is: Demand volatility hidden by averages.
What to watch: rapid swing changes in utilization between months and year prior.
Example: January: 80% total utilization February: three fully booked days — but only 77% overall utilization
Why it matters: Volatility breaks scheduling logic, weakens forecasting, and leads to staffing decisions that don’t match reality.
5. Staff Capacity Stressors
What it is: Operational drag created by turnover, vacancies, or uneven workload.
What to watch:
longer intake
increased time to room patients
slower room turns
higher documentation lag
authorization backlogs
provider frustration rising
Why it matters: Capacity drift is a leading indicator of clinical and financial underperformance.
6. Workflow Friction
What it is: Small, repeated breakdowns inside daily operations.
What to watch:
recurring PA failures
repeated coding corrections
delays at check-in/rooming/checkout
chronic “chart carryover”
Why it matters: Workflow friction compounds into denials, burnout, lost revenue, and patient dissatisfaction — often before leadership notices.
7. Patient Leakage Risk
What it is: Signals that patients may be seeking care outside your clinic.
What to watch:
longer TNAA combined with stagnant volume
no-shows rising despite reminders
missed opportunities in acute access
chronic care patients seeking online alternatives
Why it matters: Leakage is revenue that never appears on your reports.
It usually emerges when multiple earlier patterns drift at the same time.

How Patterns Support Adaptive Strategy
Patterns reveal when assumptions are aging. They make the invisible visible. This is how clinics prevent the Assumption Gap from widening throughout the year.
Clarity → see drift early
Insight → understand why it matters
Action → adjust before damage builds
Results → stability, reliability, control
Patterns are how strategy stays alive inside a busy clinic.
How to Run Your Monthly Pattern Review (20 Minutes)
Start with a By-Exception Summary
What meaningfully deviated this month?
Scan the 7 Patterns
Which signals moved?
Which assumptions weakened?
Name the single highest-risk drift (access, payer, complexity, demand, workflow, capacity, leakage)
Choose one or two targeted adjustments
Small corrections now prevent major problems later.
Follow up next month
Strategy is adapting not reacting.

Next Week
Stop Fixing Symptoms — How BI Reveals Root Causes in Your Clinic. Lean thinking meets BI.
The most powerful blog in the series.
TriStar Business Intelligence is here to help. We can help turn the noise into signal that builds your clarity and helps you to act wisely.
Contact us today and we get your free dashboard and executive summary. We customize it for your specialty and size.
Purchase our playbooks on Amazon Kindle
TriStar BI — Clarity → Insight → Action → Results








Comments